Unlock the mystery of your digestive system!
In this edition, we explore the vital roles of digestion and nutrient absorption, essential for maintaining health. Digestion is the process by which foods are broken down into smaller molecules, or nutrients, making them ready for absorption into the bloodstream. Absorption is the next step, where these nutrients are transferred from the digestive tract into the body for use. Digestion begins in the mouth and continues through the intestines, forming a highly coordinated system!
At the center of this process is the intestinal barrier, a crucial gut component that manages nutrient passage and protects against harmful substances. If gut barrier function or intestinal permeability is compromised, nutrient absorption may suffer, leading to health issues. The intestinal barrier isn’t just a gatekeeper; it’s a dynamic system that maintains balance, ensuring that nutrients are absorbed while keeping toxins out.
How nutrient absorption works: the role of the intestinal barrier and gut permeability
The role of the intestinal barrier
The intestinal barrier is formed by the mucosal layer, which separates the luminal contents and microbiota of the gut from the body’s extracellular environment. This single layer of epithelial cells includes several specialized cell types, each crucial for gut protection and nutrient absorption:
1. Enterocytes
The primary absorptive cells that transport digested nutrients into the bloodstream.
2. Goblet cells
Secrete mucus, forming a protective barrier to shield the gut lining from pathogens and mechanical damage.
3. Enteroendocrine cells
Release hormones that regulate digestion and gut motility, supporting gut health.
4. Paneth cells
Protect against infection by releasing antimicrobial peptides and enzymes that help maintain immune balance in the gut.
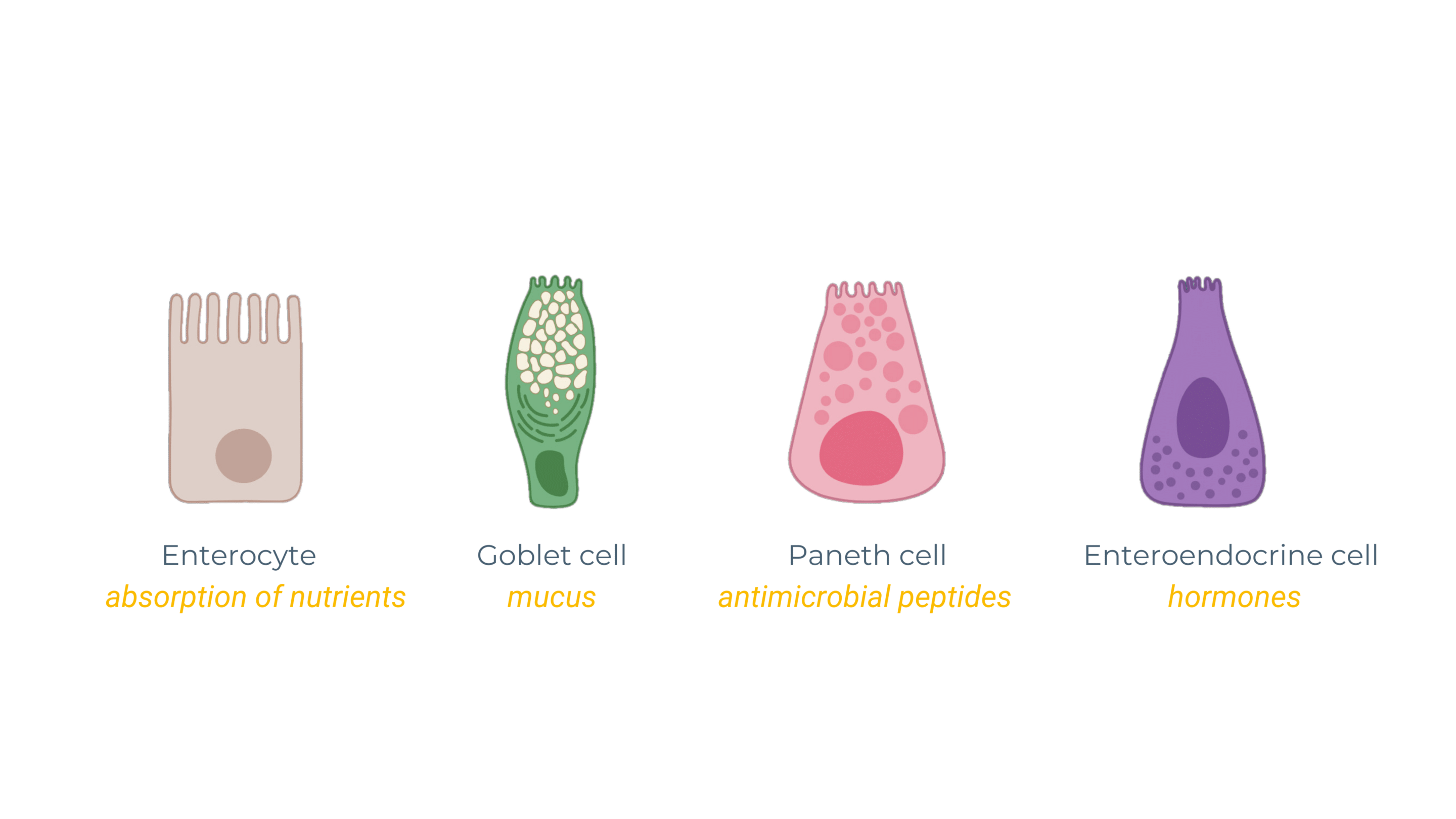
These cells collectively form the mucosal epithelial layer, supporting both nutrient absorption and the integrity of the intestinal barrier by carefully regulating intestinal permeability.
The importance of surface area in absorption
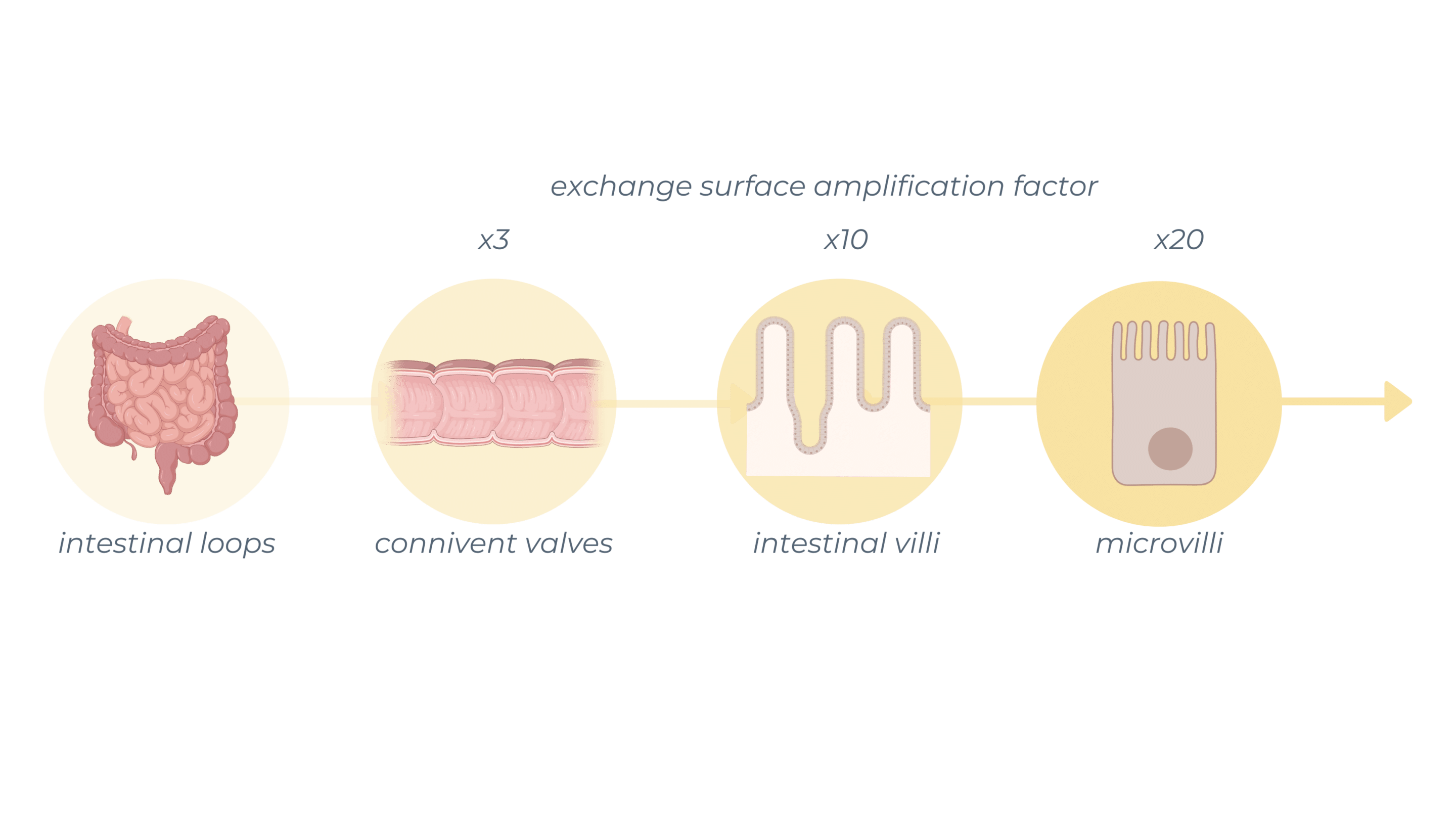
The gut’s 3D architecture, with folds, villi, and microvilli, significantly increases the surface area, optimizing interaction with the digestive contents and enhancing nutrient uptake. This design provides a large exchange area with the food bolus, which facilitates efficient absorption.
Different types of transport across the intestinal wall
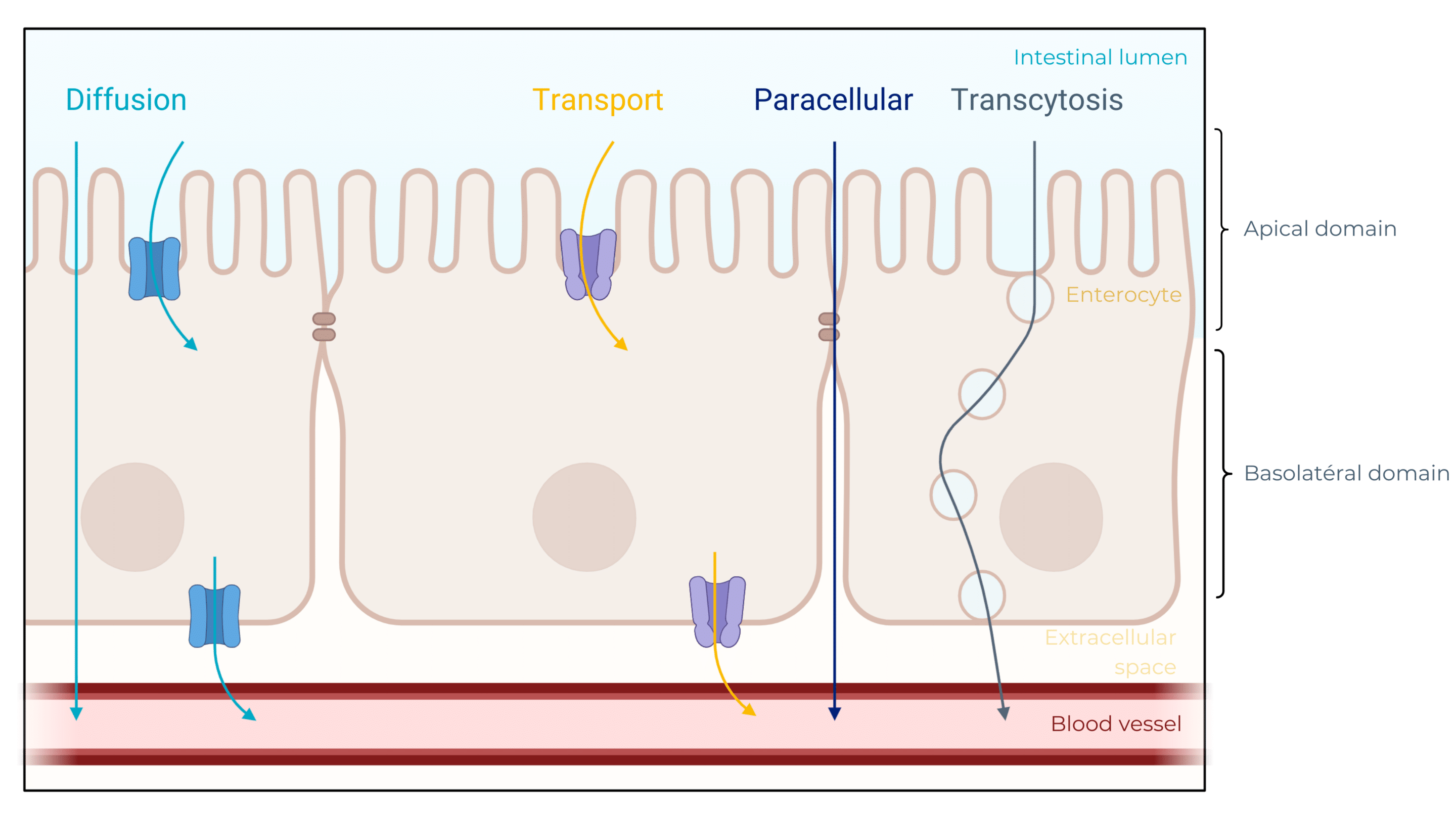
Nutrients cross the intestinal barrier through several transport methods, including diffusion, active transport, transcytosis, and paracellular transport. Each nutrient type—carbohydrates, proteins, or fats—follows a unique absorption path into the bloodstream, supporting the body’s energy and non-energy needs.
Why study the intestinal barrier? A central role in disease development
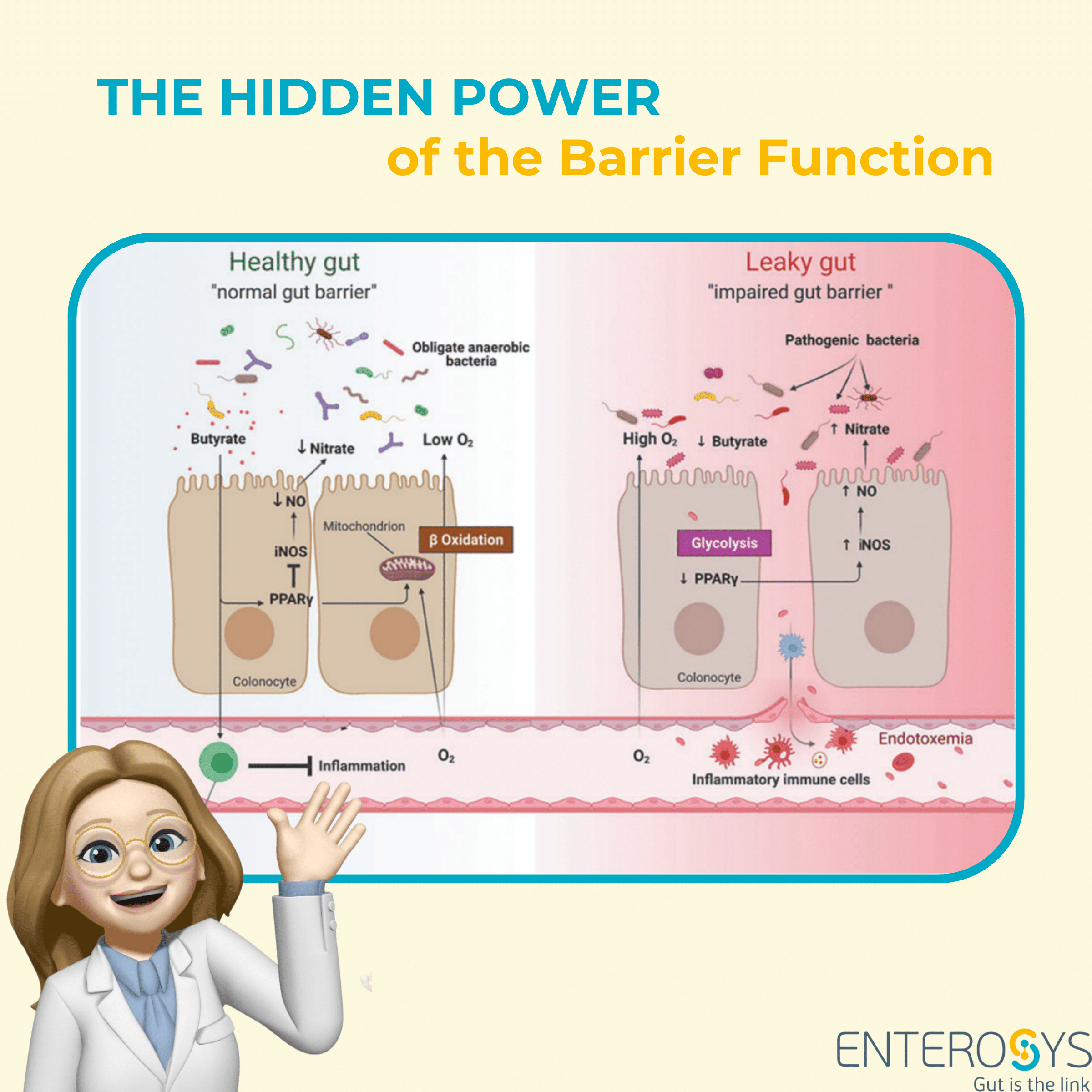
The gut is central to health. When the intestinal barrier is weakened, gut barrier disruption may lead to a range of health conditions. The immune system and inflammation are essential for maintaining this barrier, acting as a protective front line between the body and potential threats. Positioned along the intestinal mucosa, immune cells such as macrophages, T-cells, and dendritic cells monitor for harmful substances and activate an inflammatory response if needed.
However, chronic inflammation from a persistently weakened barrier can damage the gut lining, increasing intestinal permeability—a condition referred to as “leaky gut.” This allows more pathogens and harmful molecules to pass through, triggering systemic inflammation and creating a vicious cycle that is closely correlated with the development of numerous systemic conditions, including IBD, IBS, metabolic disorders, autoimmune diseases, and even neurodegenerative conditions. A balanced immune response is essential to sustain a healthy gut barrier, while unchecked inflammation can compromise its integrity and lead to far-reaching health challenges.
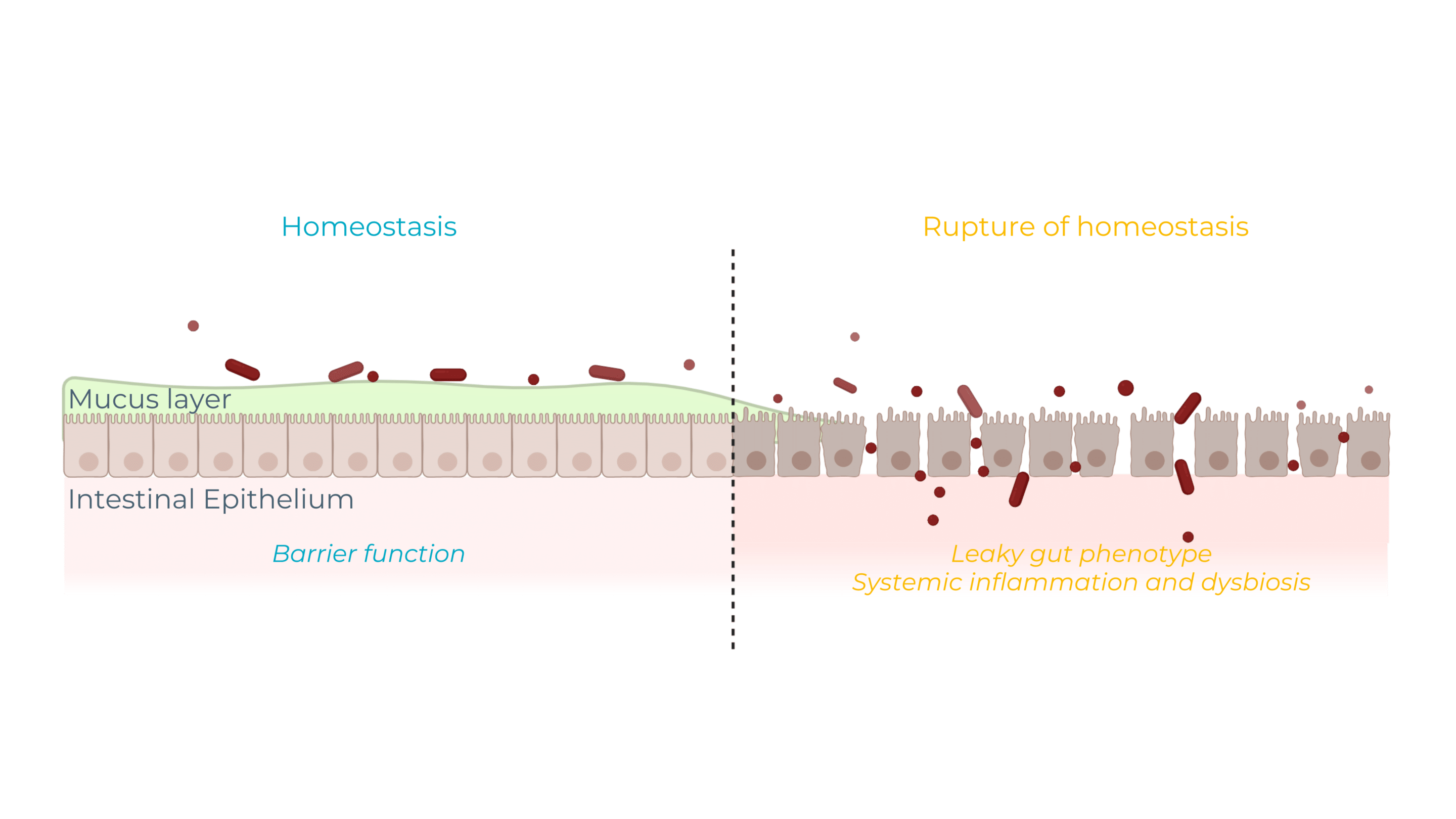
Stay tuned! In future newsletters, we’ll explore these ruptures of homeostasis mechanisms and their intricate connections with microbiota and systemic health!
Intestinal barrier and diseases
1. Inflammatory Bowel Diseases (IBD)
Chronic inflammatory diseases, including Crohn’s and ulcerative colitis, where weakened gut barrier function exacerbates inflammation and symptoms.
2. Irritable Bowel Syndrome (IBS)
A disorder characterized by abdominal pain and altered bowel habits, where increased intestinal permeability may aggravate symptoms.
3. Metabolic diseases and gut barrier function
- Type 2 diabetes – Metabolic disorder marked by insulin resistance and chronic inflammation, associated with impaired gut barrier function and systemic inflammation.
- Liver Diseases – Conditions like non-alcoholic fatty liver disease (NAFLD) and hepatitis, linked to increased intestinal permeability that allows inflammatory substances into the bloodstream, harming the liver.
4. Allergies and autoimmune disorders
Disorders like celiac disease and rheumatoid arthritis may arise when a compromised intestinal barrier allows foreign substances to enter the bloodstream, triggering chronic inflammation.
5. Neurodegenerative disorders and intestinal barrier health
Conditions such as Parkinson’s and autism are linked to gut barrier dysfunction, showing how gut health and brain function are deeply interconnected.
In upcoming editions, we’ll explore how gut health plays a role in the progression of these conditions and the physiological mechanisms at work.
Lab Chat & Latte: exploring intestinal permeability models
1. How can we study the gut barrier in vitro?
Advanced in vitro models now make it possible to study this key mechanism with precision.
From Caco-2/HT29-MTX co-cultures adding a realistic mucus barrier to sophisticated 3D models replicating crypts and villi, this article unlocks valuable insights into absorption, permeability, and immune interactions.
Read it to learn more about current models used in this field!
DOI : 10.1080/1061186X.2024.2333877
2. How the leaky gut connects to the microbiome and chronic diseases?
This article delves into the vital role of the intestinal barrier in our health and reveals how its disruption, commonly known as “leaky gut,” can trigger chronic conditions like IBD.
Conducted in humans, this study underscores several key findings: elevated intestinal permeability is strongly linked to systemic inflammation, specific biomarkers (like zonulin and LPS) provide valuable diagnostic insights, and targeted interventions such as dietary adjustments and probiotics show promise in restoring barrier integrity.
It also highlights the amplifying role of the microbiome in these imbalances.
A perfect transition to immerse you in the next newsletter, where we’ll explore the fascinating world of the microbiome and its incredible impact on our inner balance!
DOI : 10.1159/000540379
3. To go (much) further: the impact of microgravity on gut-organ axes !
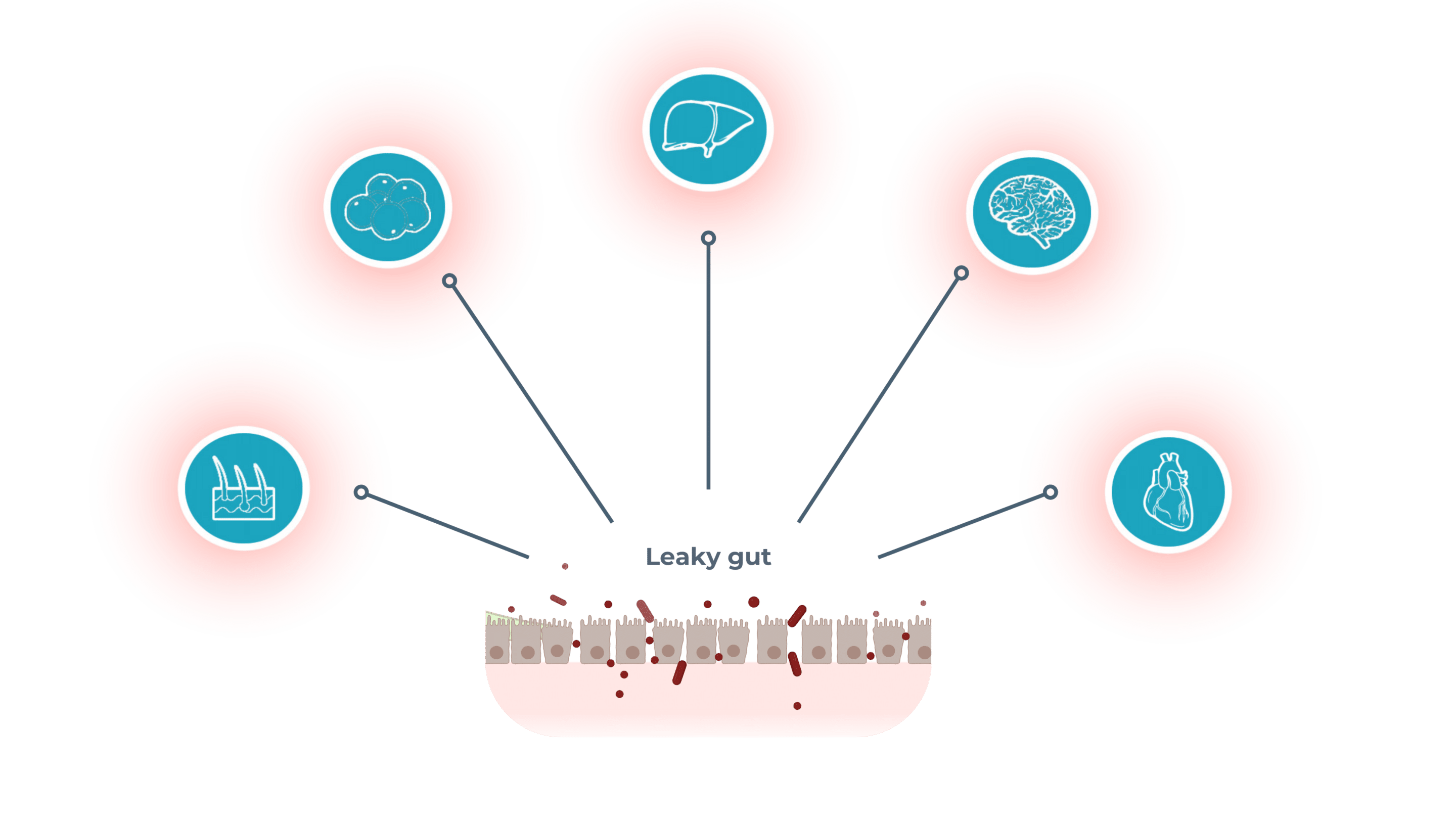
This article highlights the central role of the intestinal barrier in bidirectional communication with other organs through the “gut-organ” axes, which are essential for maintaining systemic homeostasis. Under extreme conditions such as microgravity, this barrier undergoes profound alterations, triggering a cascade of organ dysfunctions. The integrity of the intestinal barrier is therefore crucial, as its disruption affects not only intestinal physiology but also the liver, kidneys, heart, and brain, emphasizing the importance of studying these interactions to develop targeted and innovative therapeutic strategies. ts incredible impact on our inner balance!
The intestinal barrier plays a central role in systemic health, acting as a key interface between the gut and other organs. At Enterosys, we specialize in preclinical testing to explore gut-organ interactions and their impact on health. Discover how our customized in vitro and in vivo models help study complex pathologies or learn more about our expertise in gut-centric research.
Want to learn more? In the coming weeks, we’ll take a closer look at the gut’s inflammatory responses, the microbiome, and how their interplay impacts other organs. Stay with me as we reveal the many ways the gut and its microbial ecosystem influence the whole body—subscribe now to follow our journey!
Inspired by the work of Claude Knauf.