Did you know that trillions of microorganisms are working behind the scenes in your body to keep you healthy?
Often called our “hidden organ,” the gut microbiota is an extraordinary ecosystem that influences much more than just digestion.
How does this invisible community of microbes shape your immunity, metabolism, and even your mood? And what happens when this delicate balance is disrupted?
In this newsletter, we’ll uncover the fascinating world of gut microbiota: what it is, why it’s vital to your well-being, how imbalances can contribute to disease, and most importantly, how you can nurture it to unlock better health. Are you ready to explore the unseen powerhouse inside you? Let’s dive in!
What is gut microbiota?
The invisible ecosystem within us
The microbiota refers to all the microorganisms—bacteria, viruses, fungi, and archaea—that inhabit various parts of our body. While the gut microbiota is the most extensively studied due to its central role in digestion and immunity, it is only one component of a larger microbial ecosystem. Microbiota exist on the skin, in the mouth, the vagina, and even the respiratory tract. Each of these microbial communities serves unique functions:
- Skin microbiota: Acts as a protective barrier against pathogens and helps regulate immune responses.
- Oral microbiota: Plays a role in preventing dental diseases and maintaining oral health.
- Vaginal microbiota: Contributes to reproductive health by protecting against infections and maintaining a balanced pH.
- Respiratory microbiota: Helps defend against airborne pathogens and supports respiratory immunity.
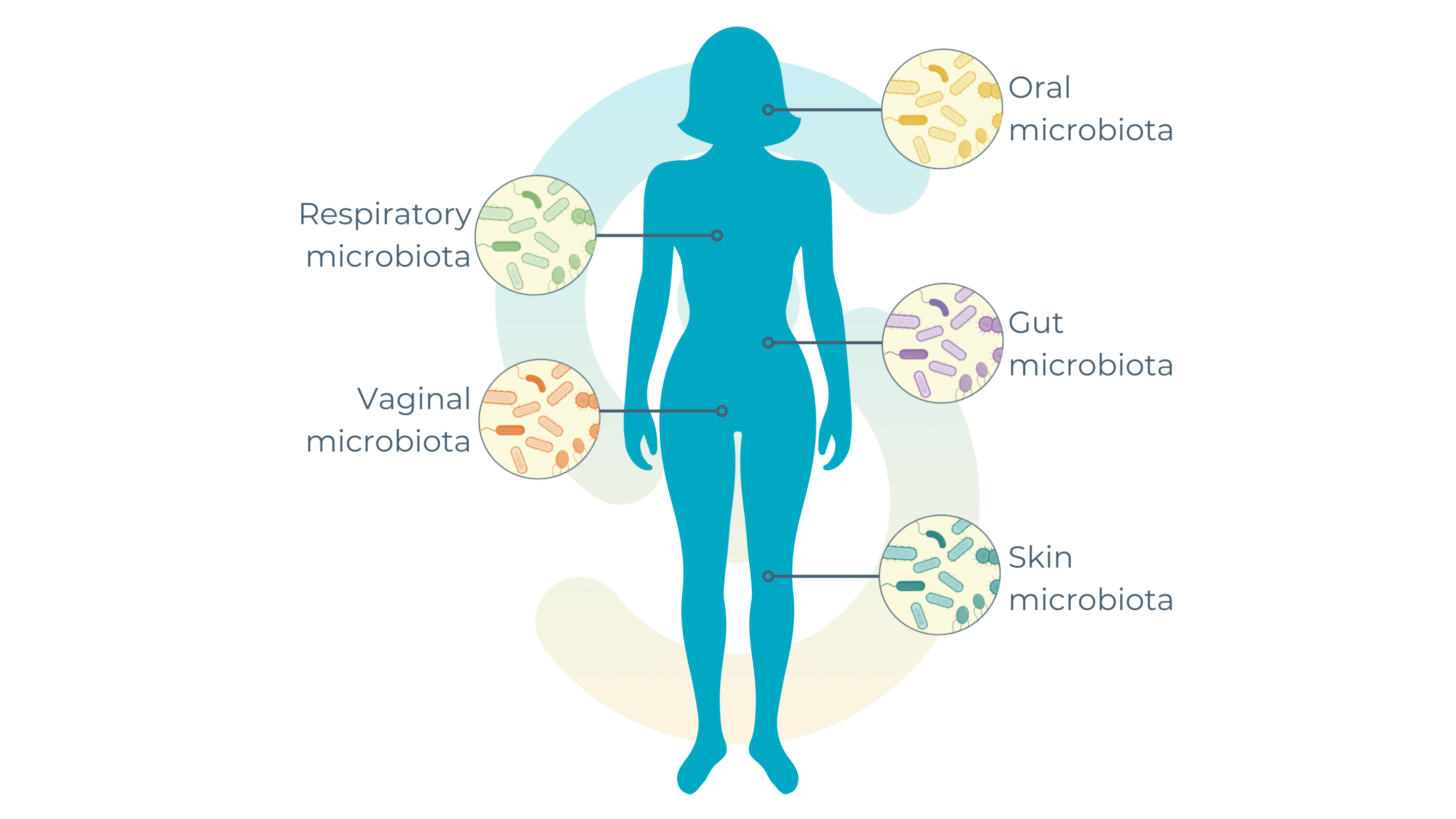
Together, these microbial communities form a dynamic network that interacts with our body, shaping health at a systemic level. However, the gut microbiota remains the largest and most diverse of these communities, often referred to as the “second genome” for its immense genetic diversity and influence on host physiology!
The symbiotic relationship between gut microbiota and host health
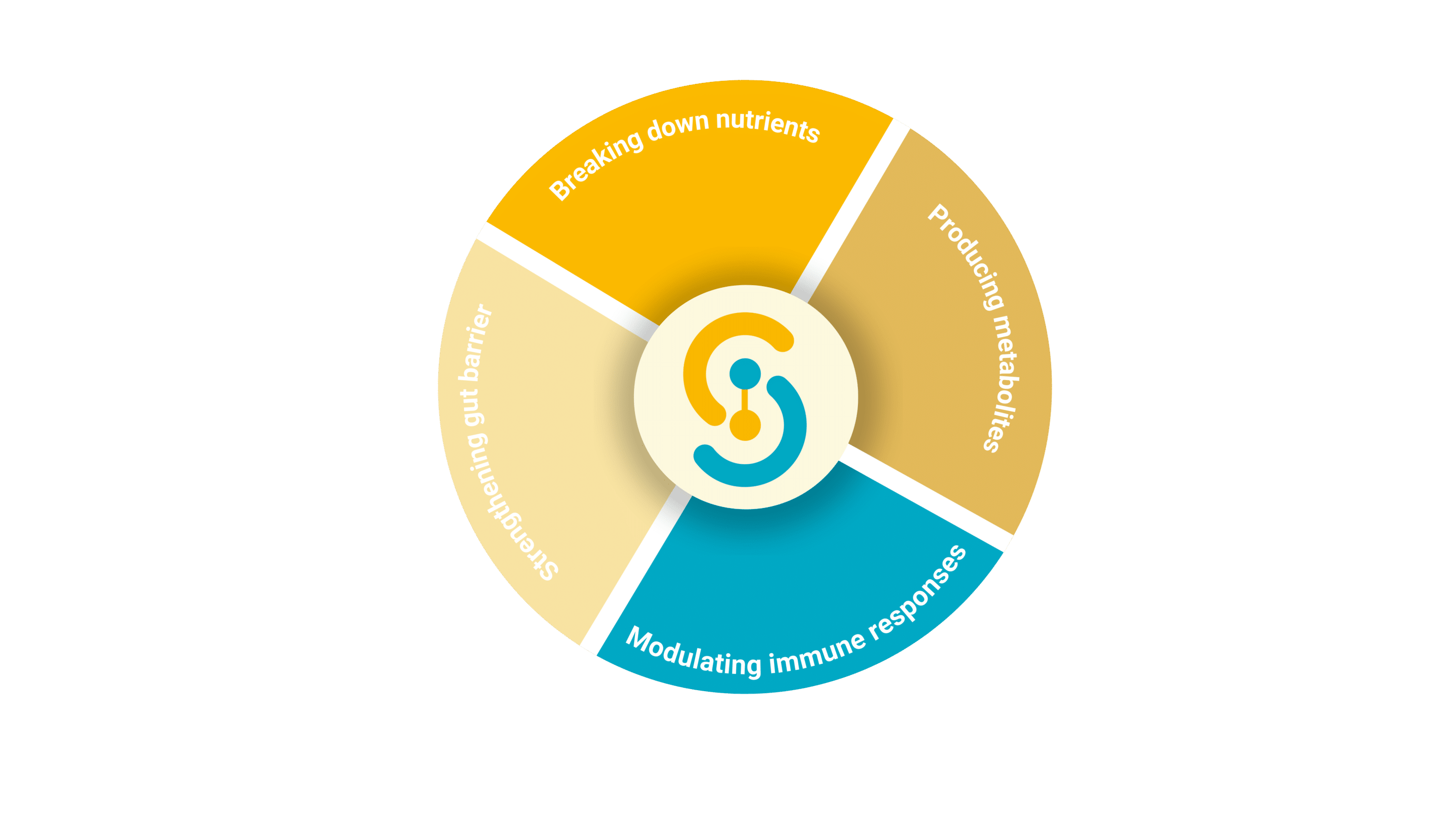
The gut microbiota plays a multifaceted role in maintaining our health by engaging in complex biochemical and physiological interactions with its host. Here’s a deeper look at its vital contributions:
1. Breaking down complex nutrients
Many dietary compounds, such as dietary fibers, resistant starches, and certain polyphenols, are indigestible by human enzymes. The gut microbiota steps in, breaking these down through fermentation processes. This generates bioactive compounds like short-chain fatty acids (SCFAs)—including acetate, propionate, and butyrate—which provide energy to colon cells, enhance nutrient absorption, and support metabolic health .
2. Producing essential metabolites
Beyond SCFAs, the microbiota synthesizes a range of metabolites with systemic effects:
- SCFAs: These molecules have anti-inflammatory properties, strengthen the gut barrier, and influence insulin sensitivity .
- Vitamins: Certain bacteria in the gut produce essential vitamins, such as biotin, folate, and vitamin K, which are critical for metabolic and blood-clotting processes .
- Bile acid derivatives: Microbial transformations of bile acids help regulate cholesterol metabolism and lipid digestion .
3. Strengthening gut barrier integrity
A healthy microbiota enhances the gut’s physical and functional barriers. SCFAs, particularly butyrate, serve as the primary energy source for colonocytes, promoting gut barrier repair and reducing intestinal permeability.
4. Modulating immune responses
The gut microbiota plays a crucial role in regulating the inflammatory response by maintaining a balance between immune tolerance and defense activation, thereby helping to prevent excessive inflammation and related diseases.
The gut microbiota and immune responses
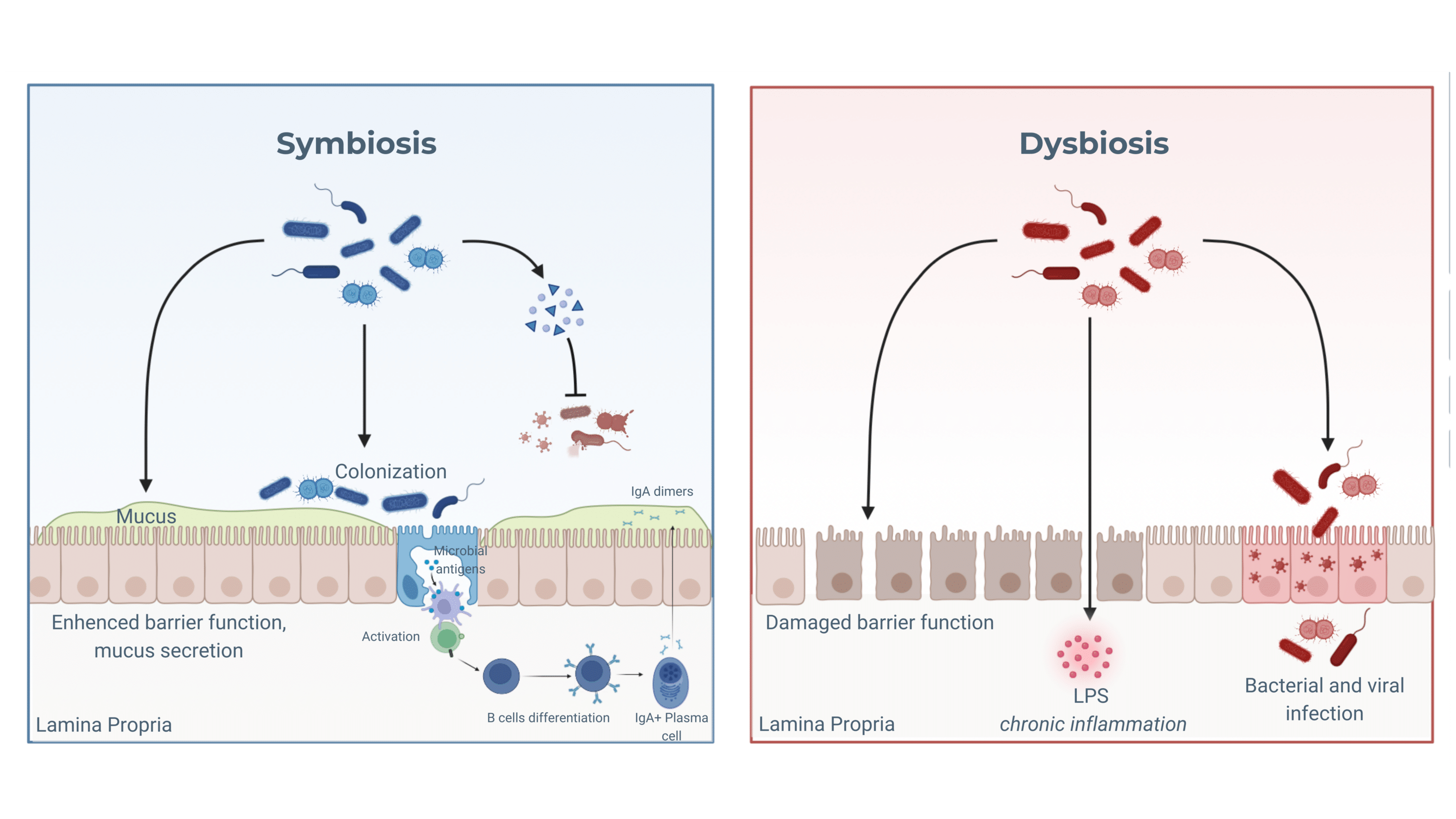
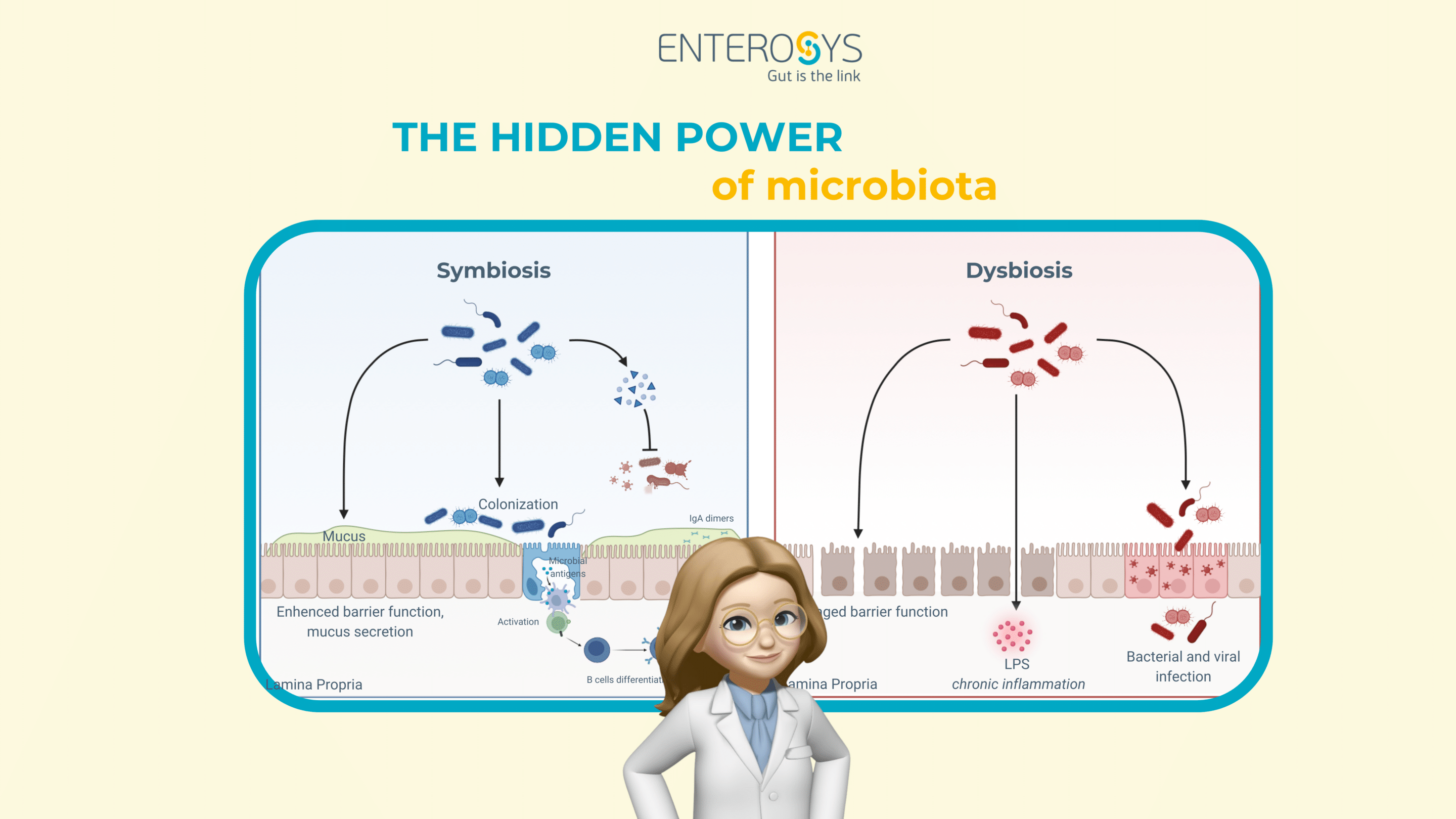
The intestinal mucosa, a complex and highly regulated structure, plays a pivotal role in maintaining immune tolerance. It consists of a mucus layer produced by goblet cells, an epithelial barrier strengthened by tight junctions, and specialized immune cells, such as dendritic cells and lymphocytes. Key players include M cells, which sense microbial antigens and transport them to underlying Peyer’s patches, initiating controlled immune responses. This architecture forms a “demilitarized zone,” where beneficial microbes thrive while potential pathogens are kept at bay .
In a state of balance, commensal microbes promote the production of anti-inflammatory cytokines, such as IL-10 and TGF-β, which support regulatory T cells (Tregs). These cells play a crucial role in suppressing excessive immune responses and ensuring that the immune system coexists peacefully with the microbiota. Additionally, the gut microbiota stimulates the production of IgA antibodies, which neutralize harmful microbes and prevent their adhesion to the epithelial surface .
However, during dysbiosis, this harmony is disrupted. A decrease in beneficial microbes and an overgrowth of opportunistic pathogens (pathobionts) compromise the epithelial barrier. This allows microbial products, such as lipopolysaccharides (LPS), to penetrate the mucosa and trigger an inflammatory cascade. Innate immune sensors detect these disruptions, leading to the recruitment of inflammatory cells and the release of pro-inflammatory cytokines like IL-6 and IL-1β .
This state of chronic inflammation can escalate into conditions such as inflammatory bowel disease (IBD) or metabolic disorders, underscoring the critical need for a balanced gut microbiota. Maintaining this balance is essential for preserving intestinal health and preventing systemic inflammation.
How to support a healthy gut microbiota
Diet and lifestyle
A fiber-rich diet, including fruits, vegetables, and whole grains, supports microbial diversity and fosters the production of beneficial metabolites like short-chain fatty acids (SCFAs), which play a key role in gut health. In addition to dietary adjustments, prebiotics (compounds that feed beneficial bacteria) and probiotics (live beneficial bacteria) are widely recognized for their ability to enhance gut microbiota composition and function.
Advanced therapies for modulation
Emerging solutions like pre, pro and postbiotics offer innovative approaches to restoring gut microbiota balance, particularly in cases of severe dysbiosis where conventional interventions fail.
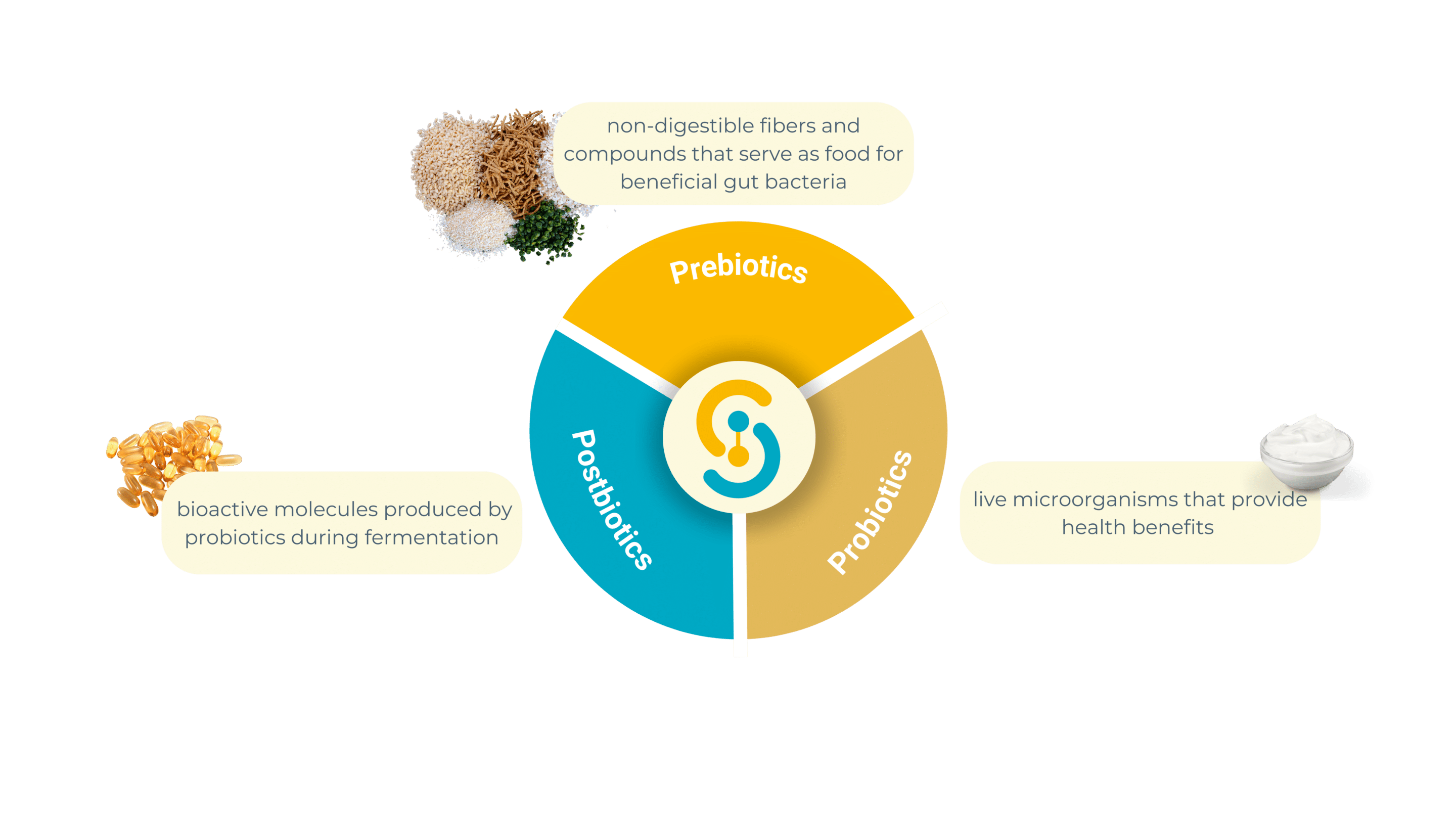
1. Prebiotics: feeding beneficial microbes
Prebiotics are non-digestible fibers and compounds that serve as food for beneficial gut bacteria. Found in foods like garlic, onions, bananas, and whole grains, they act as fuel to stimulate the growth and activity of specific beneficial microbial populations.
- Production of Short-Chain Fatty Acids (SCFAs): Prebiotics enhance the fermentation processes of gut bacteria, leading to the production of SCFAs like butyrate, propionate, and acetate, which strengthen the gut barrier and reduce inflammation.
- Improved Nutrient Absorption: By promoting a balanced microbial ecosystem, prebiotics support better digestion and nutrient assimilation.
- Immune System Modulation: Prebiotics interact with immune cells to regulate inflammatory responses and promote gut homeostasis.
2. Probiotics: live allies for gut balance
Probiotics are live microorganisms (like Lactobacillus and Bifidobacterium strains) that provide health benefits when consumed in adequate amounts. Available in fermented foods (yogurt, kefir, sauerkraut) or as supplements, probiotics directly introduce beneficial bacteria into the gut ecosystem.
- Restoring Microbial Diversity: Probiotics replenish and stabilize gut bacterial communities, particularly after disruptions caused by antibiotics or illness.
- Gut Barrier Protection: They reinforce epithelial integrity, reducing the risk of harmful compounds crossing into the bloodstream.
- Anti-Inflammatory Effects: Probiotics produce metabolites and signals that reduce pro-inflammatory cytokines, promoting immune balance.
- Enhanced Digestibility and Bioavailability of Nutrients and Drugs: Certain probiotic strains improve the breakdown and absorption of complex nutrients and can enhance the bioavailability of medications, ensuring they are better absorbed and utilized by the body.
3. Postbiotics: bioactive compounds for precision therapy
Postbiotics are bioactive molecules produced by probiotics during fermentation. These include short-chain fatty acids (SCFAs), enzymes, antimicrobial peptides, and cell wall fragments. Unlike probiotics, postbiotics do not rely on live bacterial colonization, making them more stable and easier to standardize in therapeutic applications.
- Anti-Inflammatory Properties: Postbiotics help modulate immune responses and reduce chronic inflammation.
- Enhanced Gut Barrier Function: They strengthen epithelial junctions and support mucus production, reducing intestinal permeability.
- Systemic Health Benefits: Postbiotics influence not only gut health but also metabolic and immune pathways throughout the body.
- Improved Bioavailability of Key Compounds: Certain postbiotic metabolites can modify the chemical structure of nutrients and drugs, improving their solubility, stability, and absorption in the gut.
The need for preclinical testing
Both pro, pré, and post- biotics require rigorous preclinical testing to ensure safety, efficacy, and optimal therapeutic outcomes. Here’s why these tests are indispensable:
- Mechanistic Insights: Preclinical studies shed light on how these compounds interact with the host’s gut microbiota and immune system. For example, how a specific prebiotic fiber fosters SCFA production or how a postbiotic molecule strengthens epithelial barriers.
- Dose Optimization: Identifying the right dose and delivery method is critical. Preclinical models allow controlled experiments to fine-tune administration protocols.
- Safety Evaluation: Ensuring that prebiotics do not cause undesirable fermentations, probiotics are free from antibiotic resistance genes, and postbiotics do not trigger off-target effects is essential for safe application.Efficacy Validation: Testing in preclinical models enables researchers to evaluate therapeutic effects on key indicators like microbial diversity, inflammation markers, and gut barrier function.
- Personalized Approaches: Different individuals respond uniquely to pre-, pro-, and postbiotics. Preclinical testing helps simulate diverse physiological and pathological conditions, paving the way for tailored interventions.
Your gut microbiota is more than just a collection of microbes—it’s a powerful ally in maintaining your health. From supporting digestion to boosting immunity and reducing inflammation, it plays a critical role in your well-being. With innovations like prebiotics and probiotics leading the way, the future of gut health is brighter than ever. Contact us to know how we can help you to study this impact of your compounds on microbiota !
Curious to learn how your gut talks to your brain?
In our next newsletter, we’ll dive into the fascinating world of the enteric nervous system (ENS), often called your “second brain,” and explore its incredible connection with the microbiota. Stay tuned!
Lab Chat & Latte: test your knowledge about gut microbiota !
Gut Microbiota Quiz
Test your knowledge on gut microbiota and discover how much you know!
1. What is the primary function of short-chain fatty acids (SCFAs) in the gut?
2. Which factor has the greatest influence on gut microbiota composition?
3. Which of these compounds is NOT a product of gut microbiota?
4. Which dietary component feeds beneficial gut bacteria?
5. What factor can negatively impact gut microbiota diversity?
6. Which microbiota imbalance is often linked to obesity?
To craft this newsletter, we drew insights from these three key articles 📚✨
- Van Hul M, Neyrinck AM, Everard A, Abot A, Bindels LB, Delzenne NM, Knauf C, Cani PD. Role of the intestinal microbiota in contributing to weight disorders and associated comorbidities. Clin Microbiol Rev. 2024 Sep 12;37(3):e0004523. doi: 10.1128/cmr.00045-23. Epub 2024 Jun 28. PMID: 38940505; PMCID: PMC11391702.
- Zhang F, He F, Li L, Guo L, Zhang B, Yu S, Zhao W. Bioavailability Based on the Gut Microbiota: a New Perspective. Microbiol Mol Biol Rev. 2020 Apr 29;84(2):e00072-19. doi: 10.1128/MMBR.00072-19. PMID: 32350027; PMCID: PMC7194497.
- Van Hul M, Cani PD, Petitfils C, De Vos WM, Tilg H, El-Omar EM. What defines a healthy gut microbiome? Gut. 2024 Oct 7;73(11):1893-1908. doi: 10.1136/gutjnl-2024-333378. PMID: 39322314; PMCID: PMC11503168.